What is Plantar Fasciitis and how can it be treated?
Book a Free Intro call - T: 07500 938115, E: Mrshariff-sec@outlook.com
The Sajid Shariff clinic is the leading, private orthopaedic Kent-based clinic that can help, listen and advise on a wide range of treatments for Plantar Fasciitis. Book a free Intro call with our Medical Secretary to discuss the treatment options available.
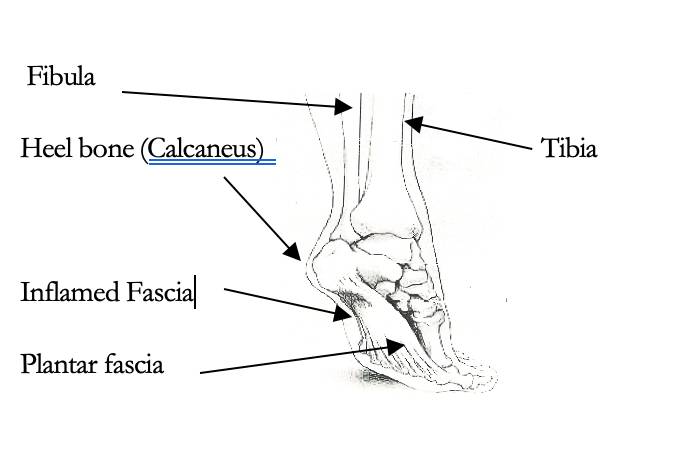
What is Plantar Fasciitis?
Book a call with one of our team
Find out how we can help you with your Plantar Fasciitis with non-surgery treatments. Simply fill in this contact form and our Medical Secretary will be in touch to schedule a time that works for you.Symptoms of Plantar Fasciitis

Testimonials
Kent’s Holistic Foot & Ankle specialists
The Sajid Shariff clinic is a private orthopaedic clinic based in SE London and Kent that specialises in surgical and non-surgical treatment of foot and ankle conditions including plantar fasciitis, ankle sprains, bunions and achilles tendonitis.

Keep an eye on the shape of your feet; if you see changes see a doctor to find out if there are any recommendations to prevent hallux valgus from forming
Use a variety of exercises to stretch your feet and calves

Try to avoid shoes that have a heel or pointed toe
Causes of Plantar Fasciitis
There are many potential causes of Plantar Fasciitis:
- Mechanical Imbalance – more common in people who spend the majority of the day on their feet. High arched feet are more at risk of developing plantar fasciitis as they are less likely to absorb the stresses of walking.
- Recent weight gain – being overweight may be a contributing factor of plantar fasciitis.
- Tightness of the Achilles tendon – this can cause stress on your heel.
- Change in activity – if you have recently changed your exercise routine e.g. increasing mileage when running, running on different surfaces or even walking on hard surfaces i.e. cement/concrete floors.
- Unsuitable footwear – if your shoes have non- cushioning soles or are worn out!
- Rheumatic conditions – if you suffer from rheumatoid arthritis or ankylosing spondylitis you may be prone to inflammation anywhere a ligament is attached to a bone. Therefore plantar fasciitis may be part of the general condition.
- Heel spurs – occasionally extra bone forms producing a small bony prominence. Many people have a bony spur on the heel bone, but this is not the cause of the pain. This may be more common in those with plantar fasciitis, but do not cause plantar fasciitis.
Treatments we offer for Plantar Fasciitis
Non Surgical Treatments
- Non-steroidal anti-inflammatory drugs (e.g. ibuprofen, nurofen)
- Appropriate footwear + Orthotics + Night splints: Use shoes with extra cushioning eg. trainers. Arch supports and or heel cushions can be used in shoewear. Night splints help to stretch the calf at night time and reduce morning pain.
- Stretching of the Calf/Gastrocnemius muscles (physio)
- Drop Stretch Exercises:
- Stand on a step – support yourself only on the front of feet, keeping knees straight. A moderate stretch of the calf muscles should be felt. Hold for 30-60seconds. If possible do on one leg for maximum weight (single leg) to stretch the muscle. Repeat 20-30 times in one go and try to perform morning and evening.
Shockwave: This is a noninvasive treatment which takes 5-10min per session, at least 3 sessions are recommended once per week. The results are much better when used with stretching exercises, on its own shockwave has minor benefit.
Injections: Steroid Injections are unpredictable but easy to administer and carry small risks of infection and damage to heel-pad tissues. These can be tried after alternative therapies have been unsuccessful. PRP injections have promising results in the literature and may have less risk but can be painful to undergo.
Surgical Treatments
Surgery is rarely required.
Results & Next steps
Over 98% of patients will have resolution of their symptoms with these treatment steps. Your symptoms may take up to 18 months to resolve. Occasionally symptoms re-occur and treatment is again necessary.
Surgery is rarely required and there are associated risks & possible complications: including infection, persistent pain and damage to the small nerves in the heel causing tingling & numbness! Division of the plantar fascia can result in a flat foot.




