Treatment for Posterior Ankle Impingement (Dancer's Heel)
Contact the clinic today to discuss your options - Email: Mrshariff-sec@outlook.com, Tel: 07500 938115
What is Posterior Ankle Impingement (Dancer's Heel)?

Causes and symptoms of Posterior ankle impingement?
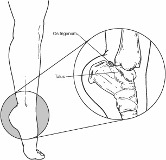
Posterior ankle impingement may be caused by bony or soft tissue structures: os trigonum syndrome, flexor hallucis longus tenosynovitis and injury to the posterior ligaments. The os trigonum is the most common cause of symptomatic posterior ankle impingement.
Common symptoms:
- Deep, aching pain in the back of the ankle, worse when pushing off on the big toe (as in walking) or when pointing the toes downward
- Tenderness in the back of the ankle
- Swelling in the back of the ankle
What is Os Trigonum Syndrome?
Most people are unaware that they have an os trigonum.
Os trigonum syndrome can be triggered by a single injury, such as an ankle sprain or caused by repetitive downward pointing of the toes, which is common among ballet dancers, soccer players and other athletes.
When pointing the toes downward, the os trigonum can become crunched between the ankle and heel bone, resulting in a “nutcracker injury.” As the os trigonum is moved, the tissue connecting it to the talus is stretched or torn and the area becomes inflamed.
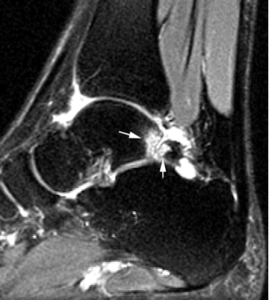
What is the Os Trigonum?
Kent’s Holistic Foot & Ankle specialists
The Sajid Shariff clinic is a private orthopaedic clinic based in SE London and Kent that specialises in surgical and non-surgical treatment of foot and ankle conditions including ankle sprains, bunions, plantar fasciitis and achilles tendonitis.
Keep an eye on the shape of your feet; if you see changes see a doctor to find out if there are any recommendations to prevent hallux valgus from forming
Strengthen your feet by exercising them

Wear shoes that fit your feet well and offer good support

Try to avoid shoes that have a heel or pointed toe
Diagnosis & Treatment for Os Trigonum Syndrome
Diagnosis
After taking a history the foot and ankle are examined, x-rays or other imaging tests (MRI scans) are often required to make the diagnosis.
Treatments for Os Trigonum
RICE (Rest, Ice, Compression, Elevation)
For milder sprains, the simple home treatment follows the RICE protocol:
RICE: Rest Ice Compression Elevate
- Rest the ankle by not walking on it.
- Ice should be applied as soon as possible to keep the swelling down. Use it for 20 to 30 minutes, three or four times daily. Do not apply ice directly to the skin.
- Compression dressings or bandages will support the injured ankle.
- Elevate the ankle above the level of your heart as often as possible during the first few days.
Medication: Nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen and naproxen can help control pain and swelling.
Non Surgical Treatments
Some sprains will require treatment in addition to the RICE protocol and medications.
- Treatment: Non-surgical Approaches
Relief of the symptoms is often achieved through treatments that can include a combination of the following:- Immobilization. A walking boot can be used to restrict ankle movement and allow the injured tissue to heal.
- Physiotherapy
- Pain relief medication. Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, may be helpful in reducing the pain and inflammation.
- Injections. Steroid/Cortisone is injected into the area to reduce the inflammation and pain.
- Strengthening exercises, such as toe-raising, are too painful. Exercises with resistance are added as tolerated.
- Proprioception (balance) training. Poor balance often leads to repeat sprains and ankle instability. A good example of a balance exercise is standing on the affected foot with the opposite foot raised and eyes closed. Balance boards are often used in this stage of rehabilitation.
- Endurance and agility exercises. Once you are pain-free, other exercises may be added, such as agility drills. Running in progressively smaller figures-of-8 is excellent for agility and calf and ankle strength. The goal is to increase strength and range of motion as balance improves over time.
When is Surgery Needed?
Most patients improve with non-surgical treatment. If the pain persists the surgery may be required to relieve the symptoms. Surgery typically involves removal of the os trigonum, as this extra bone is not necessary for normal foot function.
Other types of Posterior Ankle Impingement
Posteromedial impingement: Following injury to the Posterior Tibiotalar ligament
Posterolateral impingement: Following injury to the Posterior Talofibular Ligament (PTFL)

